By Insha Qari
In late December 2019, several local health facilities reported clusters of patients with pneumonia of unknown causes that were epidemiologically linked to a seafood and wet animal wholesale market in Wuhan City, Hubei Province, central China. The disease subsequently spread to all provinces of China and 164 countries and territories around the globe. Among the deaths in Wuhan, the noted victims of the virus include the Chinese doctor who tried to warn about the spread of “SARS-like” virus, Li Wenliang, as well as Liu Zhiming, the hospital director.
Coronavirus
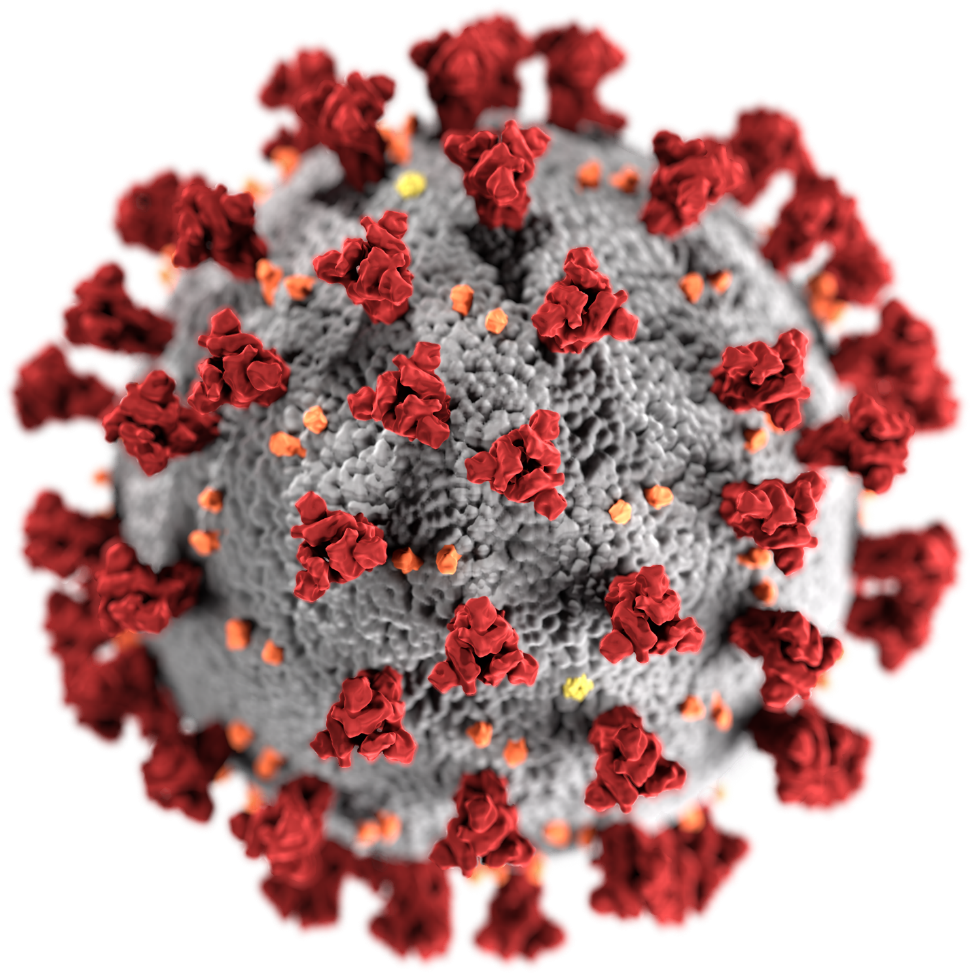
The name coronavirus comes from the Latin word corona, meaning crown or ring of light referring to the shape of the virus under an electron microscope. Coronaviruses have crown-like spikes on their surface (Figure 1.). These spikes are viral glycoproteins required for attachment at the host cell surface. Once attached, the viral membrane can fuse itself to the cell membrane, gaining entry and starting the infection. Coronaviruses are enveloped viruses having positive-sense single-stranded RNA of approximately 30,000 bases in length. These viruses are distributed broadly among humans, animals (including camels, cats, and bats) and birds causing respiratory, enteric, hepatic, and neurologic diseases.
Human coronaviruses were first identified in the mid-1960s. Seven coronaviruses can infect people. Four viruses 229E, OC43, NL63, and HKU1 are prevalent and typically cause common cold symptoms in people. The two other strains Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) and Middle East Respiratory Syndrome Coronavirus (MERS-CoV) have been linked to severe pneumonia and bronchiolitis, and sometimes fatal illness. The cause of the current outbreak is the new 7th coronavirus, the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), previously called the 2019 novel Coronavirus (2019-nCoV). This is the origin of the ongoing coronavirus outbreak, that the World Health Organization officially designated as Coronavirus disease-19 (COVID-19). The disease was designated a Public Health Emergency of International Concern by the WHO like polio in 2014, Ebola in 2014, Zika in 2016 and Ebola again in 2019. On March 11, 2020, WHO declared COVID-19 pandemic, raising the health emergency to its highest level. At that time there were about 118,000 COVID-19 cases in 115 countries, and 4,291 deaths. In the last pandemic in 2009, the H1N1 influenza “swine flu” is estimated to have killed 151,700 – 575,400 people around the globe during the first year of virus circulation (Dawood et al., Lancet Infect Dis 2012;12: 687–95)
Zoonotic origin
Coronaviruses are transmitted between animals and people. The MERS-CoV transmitted from bats to humans through camels in Saudi Arabia in 2012. This pathogen was responsible for severe respiratory disease outbreaks in 2012 in the Middle East. There were about 2,494 cases of MERS in 27 countries including 2 US cases, with about 858 deaths (WHO, Nov 2019). The fatality rate was more than 34.4%.
The SARS-CoV transmitted from horseshoe bats to humans through civet cats in China in 2002. It was the agent responsible for the SARS outbreaks in 2002 and 2003 in Guangdong Province, China. SARS infected 8,098 people, including 27 in the US, resulting in 774 deaths reported in 17 countries. The fatality rate was less than 10%.
The SARS-CoV-2 genome is about 96% identical to a bat coronavirus indicating that it may have originated in bats. A group of researchers found a coronavirus in smuggled pangolins that was a 99% genetic match to the SARS-CoV-2 circulating in people. In parts of China Pangolin meat is a delicacy and its scales are used in traditional medicine. It is suspected that SARS-CoV-2 may have transmitted from bat to humans through pangolins. Most of the early COVID-19 cases had contact history with the original seafood market; however, the disease has now progressed by human-to-human transmission. Globally, about 3.5% of reported COVID-19 cases have died. By comparison, the seasonal flu fatality rate in the US during 2018-19 influenza season was about 0.1% (more than 35.5 million illnesses, 34,200 deaths).
Symptoms
The SARS-CoV-2 infects the epithelial cells within the lungs causing mild to severe respiratory illness with symptoms of fever, cough, runny nose, shortness of breath and breathing difficulties. In more severe cases, it can lead to pneumonia, multiple organ failure, and even death. Fever may not be present in some patients. Because of the similarities of these symptoms with other related diseases, laboratory tests are required to confirm if someone has SARS-CoV-2. Current estimates of the time between infection and the onset of clinical symptoms of the disease range from 1-14 days. Most infected people show symptoms within five to six days, but there have also been cases where patients were asymptomatic despite having the virus in their system. People who are older or have existing medical conditions, such as asthma, heart disease, cancer, and diabetes may be at higher risk of serious illness. According to the WHO’s recommendations, individuals who have been in contact with confirmed coronavirus patients should be monitored for 14 days.
Morbidity and mortality
The SARS-CoV-2 infection status across the globe continues to change quickly and morbidity and mortality reports presented in this article will be outdated soon. As of March 17, 2020, the coronavirus COVID-19 is affecting 164 countries and territories around the world and one cruise ship. There were total 197,467 cases reported of which 81,691 have recovered and 7,953 died. Most of the affected countries include China (3,226 deaths out of 80,881 total cases), Italy (2,503 out of 31,506), Iran (988 out of 16,169), and Spain (533 out of 11,748). The first infection with SARS-CoV-2 in the United States was reported on January 21, 2020, and so far, there have been 6,084 cases and 101 deaths. These include imported cases in travelers, cases among close contacts of a known case, and community-acquired cases where the source of the infection is unknown. The current count of cases of infection in the United States is available on the designated website of the Centers for Disease Control and Prevention (CDC). The country-wise current number of new cases, total cases, new deaths, total deaths, active cases, total recovered cases, and serious cases are available at https://www.worldometers.info/coronavirus/.
Prevention
SARS-CoV-2 can spread from one person to another, most likely through droplets of saliva or mucus carried in the air for up to 6 feet or so when an infected person coughs or sneezes. Viral particles may be breathed in or land on surfaces that then people touch and transfer the virus further with shaking hands or touching other objects.
There is currently no approved vaccines to prevent infection with SARS-CoV-2. Scientists around the globe are racing to develop a vaccine, which will then be tested in trials. A vaccine called mRNA-1273 developed by NIAID scientists and their collaborators at the biotechnology company Moderna, Inc. in Massachusetts is currently being tested on volunteers. It could be some time before a vaccine against SARS-CoV-2 infection is ready. COVID-19 is a viral disease, therefore antibiotics cannot be used as a means of prevention or treatment. At present, there is no specific antiviral treatment recommended for COVID-19 Management of COVID-19 has mainly focused on infection prevention, case detection and monitoring, and supportive care, such as medicine to reduce fever, supplemental oxygen, or respirator for critically ill patients.
However, a potential drug target has been identified in a newly mapped protein of SARS-CoV-2 called Nsp15. This protein is essential in its lifecycle and virulence. The protein is conserved among coronaviruses and is about 89% identical to that of SARS-CoV. The studies in 2010 with SARS-CoV revealed that inhibition of Nsp15 can slow viral replication. This suggests that drugs designed to target Nsp15 could be developed as effective drugs against COVID-19. The scientists also suggest that drugs in development to treat the earlier SARS outbreak could now be developed as effective drugs against COVID-19.
Although the path to drug development is still underway, there are other ways to combat the virus in the meantime. Coronavirus is an enveloped virus, meaning it is one of the easiest types of viruses to kill with the appropriate disinfectant products. The US Environmental Protection Agency has released a long list of disinfectants for use against COVID-19.
The best ways to prevent COVID-19 are to avoid being exposed to this virus and practicing personal hygiene. People frequently touch their eyes, nose, and mouth without even realizing it. Therefore, it is important to wash hands often with soap and water for at least 20 seconds to remove germs. If soap and water are not readily available, any alcohol-based hand sanitizer with at least 60% alcohol can be used. The virus from unwashed hands can be transferred to other objects, like door handles, elevator buttons, handrails, tabletops, or toys, and then transferred to another person’s hands. SARS-CoV-2 may persist on surfaces for a few hours or up to several days depending on type of surface and temperature or humidity of the environment. The virus was detectable in aerosols for up to three hours, on copper up to four hours, on cardboard up to 24 hours, and on plastic and stainless steel up to two to three days. Cleaning and disinfecting frequently touched objects and surfaces using a regular household cleaning spray or wipe can kill the virus making it no longer possible to infect people. Additional healthy practices include avoiding close contact with people who are sick, avoiding touching your eyes, nose, and mouth, covering cough or sneeze with a tissue, then throwing the tissue in the trash.
CDC does not recommend that people who are well wear a facemask to protect themselves from respiratory diseases, including COVID-19. However, people who show symptoms of COVID-19 should use facemask to prevent the spread of the disease to others. The health workers and people who are taking care of someone in close settings (at home or in a health care facility) are also required to use facemasks.
Community-based interventions such as school dismissals, event cancellations, social distancing, and working remotely can help slow the spread of COVID-19. Based on the scope of the outbreak and the severity of illness, local and state officials, in consultation with federal officials when appropriate, make the decisions about the implementation of community measures. Extensive community engagement and clear public health communications are required for the implementation of such measures.
Clinical isolation and quarantine remain the most effective means to prevent the spread of this virus. People should call their healthcare professional if they think may have been exposed to COVID-19, develop symptoms, have been in close contact with a person known to have COVID-19, or if they live in or have recently traveled to an area with the ongoing spread. The healthcare professionals work with the state’s public health department and CDC to determine if the patient needs to be tested for COVID-19. For COVID-19 patients, the CDC has provided specific guidance about prevention of further spread of the disease that include staying home except to get medical care, covering coughs and sneezes, cleaning hands often, avoiding sharing personal household items, cleaning all “high-touch” surfaces every day, monitoring symptoms, and discontinuing home isolation in consultation with healthcare providers.
Detection
Nucleic acid testing of patient samples e.g., saliva, or nasal, oral swabs is the “gold standard” for the detection of SARS-CoV-2. The test is conducted using a kit for Reverse Transcription-Polymerase Chain Reaction (rRT-PCR) to look for tiny sections of the RNA of the virus. However, these tests cannot identify people who went through an infection, recovered, and cleared the virus from their bodies. Serology testing, on the other hand, looks for the previous and recent infections by detecting in blood the antibodies (IgG, IgM) that the body has produced to fight the SARS-CoV-2. It can take about a week before the body produces ample antibodies. Serological testing is vital for surveillance and investigational purposes. A serological test can detect antibodies even if a patient has recovered, whereas a PCR test can detect the virus only if the person is currently sick.
Conclusions
In less than 20 years, SARS-CoV-2 is the third coronavirus that has crossed species to infect human populations. Several other known coronaviruses are circulating in animals that have not yet infected humans. Novel coronaviruses will likely emerge periodically in humans due to increasing human-animal interface activities, cross-species infections and the genomic recombination within coronaviruses. To ensure a rapid and successful response in the future, there is a need to improve surveillance around the globe for timely identification of any emerging and reemerging pathogens, enhance the capabilities to quickly develop and manufacture new diagnostic kits and medical countermeasures, strengthen healthcare systems to treat a large number of patients in an epidemic, and strengthen the International Health Regulations to ensure that outbreaks are identified and stopped at their source. COVID-19 is an emerging disease and there is more to learn about its transmissibility, severity, and other features. Meanwhile, staying informed from reputable sources like the CDC and WHO, practicing personal hygiene, and developing healthy habits are easy and effective ways to prevent infection with the known and unknown pathogens.
Note: This article has been compiled using the information available at reliable sources like CDC, WHO, NIH, Peer-reviewed scientific articles etc.
About the Author

Insha Qari is currently enrolled at the School of Pharmacy, University of California, San Francisco and serves as a member of theHomeland Security Foundation of America Health and Human Services (HHS) Committee.
